Thyroid cancer—while relatively uncommon compared to other cancers—has seen significant advances in how it’s treated and managed. In 2025, patients and clinicians alike have more refined tools, updated guidelines, and a greater emphasis on individualized care than ever before. In this post, we’ll walk through what you need to know about thyroid cancer treatment today: the types, the treatment options, the major guideline updates, and what that means for you or someone you care about.
1. A Quick Overview of Thyroid Cancer Types
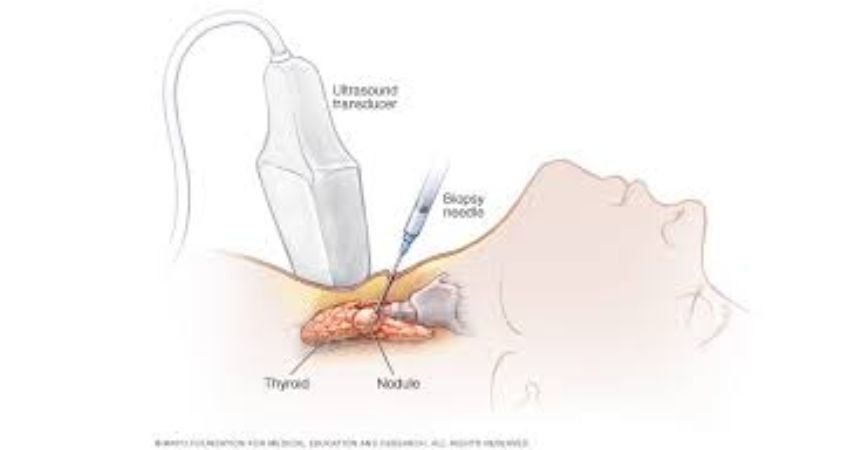
The thyroid gland sits at the front of your neck and produces hormones that regulate metabolism, heart rate, and many other body functions. When a malignant (cancerous) growth occurs in or around it, that’s thyroid cancer. The most common types include:
- Differentiated thyroid cancers (DTC): These include the papillary and follicular types (also oncocytic). They are the most frequently diagnosed thyroid cancers and generally have good prognosis.
- Medullary thyroid cancer (MTC): A less common form, arising from the thyroid’s C-cells, often with a genetic component.
- Anaplastic thyroid cancer: Rare and more aggressive.
Treatment strategies depend heavily on the type, stage (how far it’s spread) and molecular features (genetic changes) of the tumour.
2. Treatment Modalities: What’s on the Table
Here are the main approaches being used in 2025, often in combination:
Surgery
For most thyroid cancers, surgery is the first major step. This could be a lobectomy (removal of one thyroid lobe) or a total thyroidectomy (removal of the entire gland) depending on tumour size, spread, risk factors. For example, when a tumour is larger than 4 cm, research has shown worse outcomes if only lobectomy is done.
Radioactive Iodine (RAI) Therapy
For many differentiated thyroid cancers (which absorb iodine), RAI is used after surgery to destroy any thyroid tissue or tiny cancer remnants. However, its use is becoming more selective as risk-stratification improves.
Thyroid Hormone Therapy
After the thyroid is removed (in full or partly), hormone replacement (levothyroxine) is necessary. Also, in thyroid cancer, the hormone therapy may aim to keep thyroid-stimulating hormone (TSH) low to reduce the chance of cancer growth.
Radiation / External-Beam Therapy
In certain cases (e.g., non-iodine‐absorbing cancer, more advanced disease), external radiation may be used.
Targeted Therapy & Systemic Treatment
One of the most important developments in recent years: for cancers that are refractory (not responsive) to RAI or that have spread widely, targeted drugs (tyrosine-kinase inhibitors, MKIs) and other systemic therapies are increasingly used. For instance, the 2025 guidelines recommend use of drugs such as Lenvatinib or Sorafenib for RAI-refractory differentiated thyroid cancer (RAIR-DTC). Guideline Central+1 Also, molecular testing (for fusions or mutations like NTRK, RET, BRAF) is now more standard, guiding which targeted therapy should be used.
Active Surveillance / Watchful Waiting
For very low-risk thyroid cancers (especially very small papillary cancers), some clinicians now recommend careful observation rather than immediate aggressive treatment. This is part of an effort to avoid overtreatment and preserve quality of life.
3. What’s New in 2025: Guideline Updates & Key Shifts
2025 brings important updates that patients should be aware of:
- The American Thyroid Association (ATA) released major new guidelines for adult patients with differentiated thyroid cancer. These emphasize better stratification of risk, more molecular testing, and tailoring treatment intensity accordingly.
- Key changes include stronger use of genetic/molecular testing (to check for actionable drivers like NTRK/RET/ALK fusions or BRAF V600E) before systemic therapy in RAIR-DTC.
- The 2025 National Comprehensive Cancer Network (NCCN) Guidelines (version 1.2025) also emphasise systemic treatment algorithms — for example, lenvatinib or sorafenib as preferred first-line in RAI-refractory cases.
- The trend is toward de-escalation of treatment for low-risk disease: smaller operations, less use of RAI in very low-risk patients, more surveillance approaches.
- Guidelines from China for management of RAI-refractory DTC (2025 edition) showcase global alignment toward targeted therapy and precise management.
4. What This Means for You (or a Loved One)
Here are some practical implications:
- Ask about molecular testing: If your tumour is more advanced, recurrent, or refractory to standard therapy, ask your oncologist or endocrinologist whether genetic testing was done (for NTRK, RET, BRAF, etc). It may open up additional targeted treatment options.
- Understand your risk level: Not all thyroid cancers carry the same risk. Tumour size, spread to lymph nodes, whether it absorbs iodine, whether high-risk features are present — all of these influence treatment intensity. For example, a tumour >4 cm had worse outcomes in one study.
- Consider less aggressive options if you qualify: If you have a very small, low-risk cancer (e.g., papillary <1 cm, no spread), you may be eligible for lobectomy instead of total removal, or even active surveillance.
- Be aware of systemic therapy options: If the disease is not responsive to traditional treatments (surgery + RAI), targeted drugs (like lenvatinib, sorafenib) and immunotherapy in selected cases are now part of the standard of care.
- Think about long-term quality of life: Side-effects matter. Hormone replacement after thyroid removal, risks of low calcium if parathyroids are damaged, and the long-term consequences of systemic therapy are all important. New guidelines emphasise balancing cure + life quality.
- Stay connected with your care team: Because the field is evolving and guidelines are changing, you want an endocrinologist and/or oncologist who stays current and is comfortable discussing newer therapies, molecular testing, and offering nuanced advice.
5. Final Thoughts
In 2025, treatment of thyroid cancer is more individualised than ever. While many patients will still do very well with conventional approaches (surgery + maybe RAI + hormone therapy), others—particularly those with more advanced or unusual disease—now have real options beyond “one-size-fits-all”. The shift toward molecular-driven therapy, targeted drugs, and risk-based treatment intensity means you have grounds to ask questions, seek second opinions, and understand the rationale behind your treatment plan.
If you or someone you know is facing a diagnosis of thyroid cancer, it’s a good time to discuss with the care team:
- What is the exact type and stage of the cancer?
- Was molecular/genetic testing done on the tumour?
- What treatment options are being proposed and why?
- Are you eligible for less aggressive treatment (if low risk)?
- What are the side-effects, long-term consequences, and monitoring plan?
Remember: no two cases are alike. Advances in 2025 give hope, but decision-making remains deeply personal. If you’d like to dig into a specific subtype (e.g., medullary thyroid cancer, anaplastic thyroid cancer) or treatment (the specific targeted drug options, side-effect profiles) I’d be happy to help with that too.